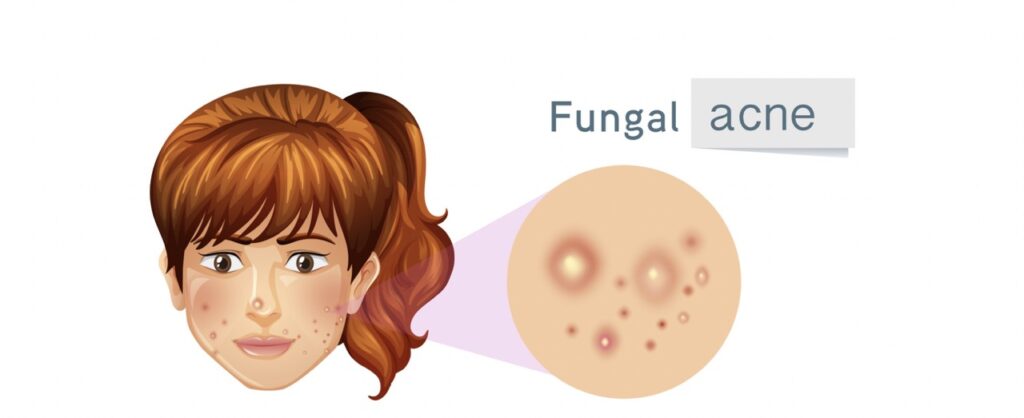
Have you ever noticed those pesky bumps on your skin that just don’t seem to respond to regular acne treatments? You may have a condition called fungal acne. Don’t worry, we’re here to break it down for you in simple terms and help you learn how to treat it effectively.
What is fungus Acne?
Fungal acne isn’t your typical acne. It’s caused by an overgrowth of yeast on your skin, and it can look a bit different from the usual pimples. Instead of the usual redness and inflammation, fungal acne often appears as tiny, uniform bumps that can be itchy or uncomfortable.
Why Understanding Fungal Acne Matters
Knowing the difference between fungus acne and regular acne is crucial because they require different approaches to treatment. If you treat fungal acne like regular acne, you might not see the results you’re hoping for. That’s why understanding what you’re dealing with is the first step towards healthier skin.
We’ll help you recognize its telltale signs, understand what causes it, and, most importantly, show you how to treat it naturally and effectively. By the end, you’ll have the knowledge you need to take control of your skin’s health and bid farewell to those troublesome bumps. Let’s get started on this journey to clearer, happier skin!
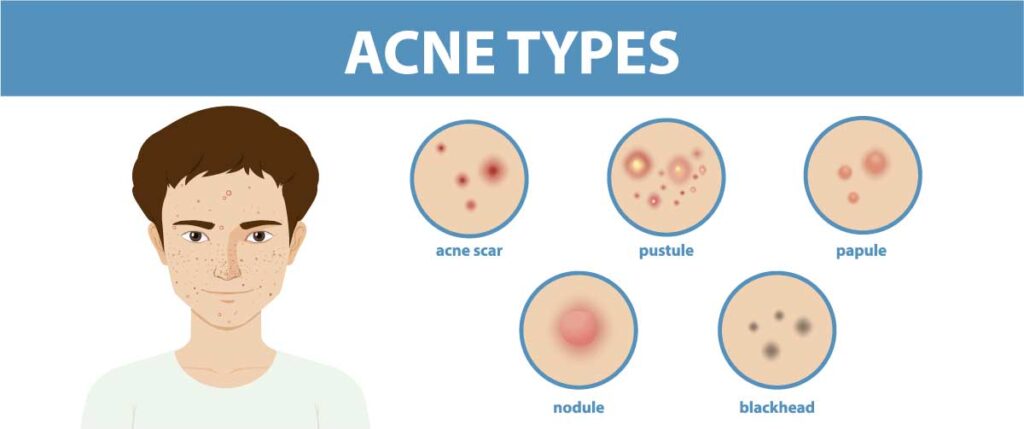
Different Types of Fungal Acne Explained
When it comes to fungal acne, it’s not all the same. Let’s break down the different kinds you might encounter:
- Malassezia folicululitis: Imagine itchy bumps that resemble acne. Blame yeast for causing these pesky papules.
- Pityrosporum Folliculitis: Think red, angry bumps thanks to yeast hanging out in your hair follicles.
- Candida Folliculitis: Here, candida yeast is the culprit, creating acne-like outbreaks.
- Pyoderma Faciale: These are the big, painful bumps, almost like pimples, caused by bacteria acting up.
Recognizing Specific Types of Fungal Acne
Each type has its own unique features. For example:
- Malassezia: Small, itchy bumps that bug you.
- Candida: Pustules that might make you think twice about your skin.
- Pityrosporum: Uniform red bumps, like a little army of them. Knowing these differences helps pick the right treatment.
Key Differences Between Fungal Acne Variations
- Appearance: Each type has its own distinct look, from red bumps to uniform ones.
- Triggers: Different things set them off. Sweat, humidity, and your skin’s pH play a role.
- Location: They’re a bit picky about where they show up. Forehead, back—they have preferences.
Understanding Fungal Acne
Fungal acne might sound puzzling, but we’re here to clear things up. It’s not your usual acne, and knowing the difference can make a big difference in how you treat it. Let’s explore and learn the fundamentals.
Defining Fungal Acne
Ever heard of fungal acne? It’s not the same as the acne you’re used to. Fungal acne is caused by a different type of critter—yeast, to be precise. This yeast, known as Malassezia, sets up shop in your hair follicles and wreaks havoc, leading to those tiny, annoying bumps that might look like regular acne but aren’t.
Busting Myths and Spotting Fungal Acne
Misconceptions about acne can leave you scratching your head, but we’re here to set things straight. Imagine thinking you’ve got stubborn pimples when it’s fungal acne. Tricky, right? So, how do you spot the difference? Fungal acne is often uniform in size, looks like a cluster of small bumps, and can appear on your back, chest, or face.
Roots of Fungal Acne
Let’s uncover what’s cooking under the surface. Humidity and sweat can provide a cozy environment for fungal acne to thrive. Using heavy moisturizers or skipping the shower after a workout? That might be giving these little troublemakers a perfect home. Lifestyle factors, like tight clothing or excessive sweating, can also contribute.
By understanding what sets fungal acne apart, you’re taking the first step in tackling it head-on. Remember, it’s not just about knowing your skin, but also understanding how these tiny yeast creatures operate. Stay tuned as we dig deeper into the realm of fungal acne and discover how to give it the boot, naturally!
What Does Fungal Acne Look Like?
Fungal acne, unlike regular acne, has a unique look that’s important to recognize. Imagine tiny, itchy bumps on your skin, resembling a rash or a cluster of pimples. These bumps can be a bit reddish, and sometimes they might even have a white or yellow top.
What Causes Fungal Acne and Factors that Make it Worse
Fungal acne happens for reasons you might not expect. Let’s dive into what makes it pop up and what habits can make it worse.
Why Fungal Acne Shows Up
Fungal acne isn’t like regular acne—it’s caused by yeasts that love warm and sweaty skin. Humid environments are like a welcome mat for these little troublemakers. When the yeasts party on our skin, they create those pesky acne bumps that we don’t want.
The Sweat Connection
Sweating is our body’s way of cooling down, but it can also be like a playground for fungal acne. When we sweat, it mixes with the natural oils on our skin, giving yeasts a perfect place to thrive. So, if you’re in a hot and humid place or you’re exercising a lot, you’re giving fungal acne a chance to join the party.
Skincare Practices that Backfire
Sometimes, the things we do to take care of our skin might be causing more trouble. Using heavy or oily skincare products can clog pores and create a cozy environment for yeast. Imagine it like a crowded room where everyone’s having a bit too much fun—that’s the kind of environment these yeasts love.
Taking Action Against Fungal Acne
If you suspect you have fungal acne, it’s good to rethink some habits. Try to keep your skin dry and clean, especially after sweating. Choose light and non-comedogenic (non-pore-clogging) skincare products that won’t feed the yeasts. And if you’re living in a humid area, consider using breathable fabrics to let your skin breathe.
Understanding and Diagnosing Fungal Acne
Fungal acne might sound strange, but it’s a skin concern that can be managed with the right knowledge. Let’s learn how to spot it and when to seek expert help.
Fungal acne isn’t your typical acne. It’s caused by yeast, not bacteria, and can look like tiny bumps or pimples. Don’t stress; we’ll assist you in figuring it out.
How to Identify Fungal Acne
- Check the Pattern: Fungal acne often appears in clusters or lines, unlike regular acne.
- Look for Itchiness: If those bumps itch more than usual, it could be fungal acne.
- Avoid Moisture: Fungal acne loves dampness, so if it gets worse in humid conditions, it might be the culprit.
- Pay Attention to Products: Certain products can worsen fungal acne. If your skin reacts to oils or heavy creams, take note.
- The Glass Test: Press a clear glass over the affected area. If the bumps disappear, it might be fungal acne.
When to Consult a Dermatologist
While home identification can help, a dermatologist is your skin’s best friend. Reach out if:
- You’re unsure about the diagnosis.
- Over-the-counter treatments aren’t working.
- The condition is spreading or worsening.
- You’re experiencing pain or discomfort.
Natural Ways to Clear Fungal Acne
Dealing with fungal acne? Good news! There are natural solutions that work wonders. We’re here to walk you through these easy and effective remedies to put your skin back on track. We have everything you need, from apple cider vinegar to tea tree oil.

Tea Tree Oil: A Tiny Solution with a Big Punch
Tea tree oil is your secret weapon against fungal acne. This natural powerhouse has antifungal properties that tackle those pesky bumps. Here’s how to use it:
- Water needs to be added to tea tree oil before use.
- Apply gently to the affected areas using a cotton ball.
- Before washing it off, give it time to perform its magic.
Apple Cider Vinegar
Apple cider vinegar isn’t just for salads; it’s a fantastic fungal fighter too.
- Water and apple cider vinegar should be combined equally.
- Apply the mixture to your skin using a cotton pad.
- Let it dry before rinsing off. It’s similar to pressing the skin’s reset button.
Aloe Vera: Soothe and Repair
Aloe vera is a soothing balm for your troubled skin. Its natural healing properties make it perfect for fungal acne recovery:
- Fresh aloe vera gel may be extracted from the plant.
- Gently apply the gel to your skin and let it absorb.
- Enjoy the calming sensation as it does its thing.
Other Natural Heroes
Don’t stop at tea tree oil and apple cider vinegar! There are more natural goodies to explore:
- Coconut oil moisturizes without clogging pores.
- Honey is nature’s antibacterial gift for your skin.
- Green tea: Sip and apply for double the benefits.
- Witch hazel: Tighten pores and say goodbye to excess oil.
Using Nizoral to Beat Fungal Acne
If you’re battling fungus, you might have heard about an unexpected hero in the fight: Nizoral, an anti-dandruff shampoo armed with antifungal powers. This unassuming shampoo isn’t just for your hair; it could be your secret weapon for achieving clear skin. Let’s dive into how Nizoral works its magic and how you can seamlessly include it in your skincare routine.
Understanding Nizoral’s Antifungal Superpowers
Nizoral’s claim to fame is its antifungal properties. While originally designed to tackle dandruff, it turns out that the same ingredients that combat those pesky flakes can also take on fungal acne. It occurs when specific yeasts go haywire on your skin, causing those frustrating breakouts. Nizoral contains an active ingredient, ketoconazole, which targets these troublemakers, helping to soothe your skin and curb those unwanted bumps.
The Step-by-Step Guide to Incorporating Nizoral
- Gentle Cleansing: Start by gently cleansing your face with a light cleanser before taking Nizoral. This ensures your skin is prepped and ready to make the most of Nizoral’s effects.
- Patch Test: It’s always wise to do a patch test before using any new product on your face. Apply a small amount of Nizoral to a discreet area of your skin and wait for about 24 hours. Start by gently cleansing your face with a light cleanser before taking Nizoral.
- Nizoral Application: Wet your face and hands, then squeeze a small amount of Nizoral onto your palms. Gently massage the shampoo onto the areas affected. Avoid getting anything in your mouth or eyes. Let it sit for about 3–5 minutes to let those antifungal powers do their thing.
- Rinse Thoroughly: After the waiting period, rinse your face thoroughly with lukewarm water. Make sure there’s no shampoo residue left on your skin.
- Follow with Care: Since Nizoral is potent, it’s recommended to use it just a couple of times a week rather than daily. On the days you don’t use Nizoral, stick to your regular skincare routine.
- Moisturize: After rinsing off Nizoral, apply a gentle, hydrating moisturizer to keep your skin balanced and happy.
Preventing Fungal Acne
Nobody likes unexpected guests, especially when they come in the form of fungal acne. But fret not; there are smart steps you can take to keep these uninvited bumps away. Let’s dive into some simple yet effective strategies to prevent fungal acne outbreaks and maintain skin serenity.
Nurturing Your Skin with Smart Habits
Maintaining healthy skin isn’t rocket science. It’s all about embracing habits that promote balance and wellness. Here’s the lowdown:
- Gentle Cleansing: Use a mild cleanser to keep your skin clean without stripping away its natural defenses. This helps prevent the buildup of excess oils that can trigger fungal acne.
- Avoid Over-Exfoliation: Scrubbing too hard or too often can disrupt your skin’s harmony. Opt for gentle exfoliation to slough off dead skin cells without irritating them.
A Hygiene Haven
Good hygiene is like a fortress against fungal acne. Follow these steps to create an environment that fungi find unwelcoming:
- Dry, Dry, Dry: After sweating or washing your face, make sure it’s thoroughly dry. Fungi love moisture, so denying them their preferred hangout is a smart move.
- Clean Towels and Pillowcases: Swap out your towels and pillowcases regularly. This reduces the chances of fungi making themselves at home.
Lifestyle Changes for Radiant Skin
Your skin reflects your lifestyle choices.
- Balanced Diet: Your skin’s health can be supported by a nutrient-rich diet. Think fruits, veggies, and plenty of hydration.
- Stress Busters: Stress isn’t a friend of clear skin. Practice relaxation techniques like deep breathing or yoga to keep stress in check.
Choosing the Right Products
The products you use play a starring role in your skin’s health story:
- Non-Comedogenic Products: Opt for skincare and makeup labeled “non-comedogenic.” These won’t clog your pores, which helps prevent acne.
- Oil-Free Products: If your skin tends to get oily, go for oil-free moisturizers and products to avoid providing extra nourishment to potential fungi.
Duration and Recovery
Dealing with fungal acne? Wondering when you’ll finally see clear skin again? Let’s dive into the timeline and factors that play a role in getting rid of those pesky fungal acne bumps.
How Much Time Does It Take to Get Rid of Fungal Acne?
On average, it might take a few weeks to notice significant improvement after starting treatment. But remember, everyone’s skin is unique, so your journey might be a bit shorter or a tad longer.
Factors That Influence Recovery Time
Several factors can affect how quickly you’ll see results:
- Severity: Mild cases might clear up faster than more stubborn ones.
- Consistency: Following your treatment routine diligently is essential for a faster recovery.
- Treatment Approach: Natural remedies and antifungal products can impact the speed of improvement.
- Hygiene: Proper skincare and cleanliness can contribute to quicker healing.
- Lifestyle: A balanced diet, staying hydrated, and reducing stress can aid in the recovery process.
When to Get Expert Help for Your Skin
If you’re struggling with persistent skin issues, it’s important to know when to turn to the pros for guidance. Here, we’ll walk you through situations where a dermatologist’s expertise is essential. Don’t hesitate to seek medical advice, especially if your case is severe or doesn’t improve.
Guidelines for Seeking Professional Dermatological Assistance
- Severe or Stubborn Cases: If your fungal acne isn’t responding to home remedies or seems unusually severe, it’s time to consult a dermatologist. They can provide specialized treatments tailored to your skin’s needs.
- Persistent Redness and Discomfort: If your skin is consistently red, itchy, or uncomfortable, it’s a sign that something might be off. Dermatologists can accurately diagnose the issue and recommend appropriate solutions.
- Unsure Diagnosis: If you’re uncertain whether your acne is fungal or not, a dermatologist can clear up the confusion. They have the expertise to identify the type of acne you’re dealing with and provide suitable advice.
Tips for Maintaining Healthy Skin and Preventing Fungal Acne
Keeping your skin healthy goes a long way toward preventing future outbreaks. Here are some easy-to-follow suggestions:
- Balanced Diet: A diet rich in fruits, vegetables, and whole grains nourishes your skin from within. Avoid excessive sugar and processed foods, which can contribute to skin issues.
- Stress reduction: Severe stress can lead to acne breakouts. Engage in activities you enjoy, practice relaxation techniques, and get enough sleep to manage stress effectively.
- Skincare Routine: Choose gentle, non-comedogenic (won’t clog pores) skincare products. Cleanse your face twice daily, and don’t forget to moisturize. Consistency is key.
Wrapping Up
In this guide, we’ve covered the ins and outs of fungal acne, from understanding it to treating and preventing it. Remember, your skin’s health matters. If you’re facing persistent issues or your symptoms are severe, don’t hesitate to reach out to a dermatologist. They’re here to help you achieve your healthiest skin.
Prioritize Your Skin’s Health and Reach Out for Help
Your skin reflects your overall well-being. If you’re uncertain about your skin’s condition or facing stubborn acne, don’t hesitate to consult a dermatologist. Their expertise can make a world of difference in achieving clear and healthy skin. Your skin deserves the best care, so make your skin’s health a priority today.
Frequently Asked Questions
Q1: What is fungal acne, and how is it different from regular acne?
Fungal acne is a skin condition caused by yeast or fungi in hair follicles, leading to itchy bumps that resemble acne. Unlike regular acne caused by bacteria, fungal acne requires a different approach for effective treatment.
Q2: What are the common types of fungal acne?
Fungal acne includes Malassezia Folliculitis, Pityrosporum Folliculitis, Candida Folliculitis, and Pyoderma Faciale. Each type has distinct characteristics and causes, which affect their appearance and treatment.
Q3: How can I identify the different types of fungal acne?
Each type has unique signs. Malassezia may cause itchy papules, Candida can result in pustules, and Pityrosporum often appears as uniform red bumps. Recognizing these differences helps in targeting the right treatment.
Q4: What triggers fungal acne outbreaks?
Factors like humidity, sweat, and an imbalance in skin pH can activate fungal acne. It thrives in warm, moist conditions, making it more common in certain environments and during sweaty activities.
Q5: Can I treat fungal acne at home?
Yes, mild cases can be treated at home. Using antifungal topicals, adjusting your skincare routine, and practicing good hygiene can help clear fungal acne. However, severe cases may require professional medical guidance.
Q6: Are there natural remedies for treating fungal acne?
Yes, natural remedies like tea tree oil and apple cider vinegar can be effective against fungal acne. However, it’s important to patch-test first and consult a dermatologist if you’re unsure.
Q7: How long does it take for fungal acne to clear up?
The duration varies based on the severity and treatment used. Mild cases might improve within a few weeks, while more stubborn cases could take several months to show noticeable improvement.
Q8: How can I prevent fungal acne outbreaks?
To prevent outbreaks, wear breathable clothing, maintain proper hygiene, and avoid excessive sweating. Following a balanced diet rich in probiotics may also contribute to skin health.
Q9: When should I seek professional help for fungal acne?
If your fungal acne is severe, widespread, or not responding to home treatments, it’s advisable to consult a dermatologist. They can provide personalized advice and prescribe appropriate medications.
Q10: Is fungal acne contagious?
No, fungal acne is not contagious. It’s caused by the overgrowth of yeast or fungi that naturally reside on the skin. However, proper hygiene is still important to prevent its development.
Q11: Can certain skincare products worsen fungal acne?
Yes, some skincare products with heavy oils or ingredients that feed yeast can worsen fungal acne. It’s best to choose non-comedogenic and fungal acne-safe products to avoid exacerbating the condition.
Q12: Can I wear makeup if I have fungal acne?
Yes, but it’s important to choose non-comedogenic and oil-free makeup products. Be sure to cleanse your skin thoroughly before and after wearing makeup to minimize the risk of worsening fungal acne.
Q13: Can stress contribute to fungal acne outbreaks?
Stress doesn’t directly cause fungal acne, but it can weaken the immune system, making you more susceptible to various skin issues, including fungal acne. Managing stress can positively impact overall skin health.
Q14: Is it possible for fungal acne to recur after treatment?
Yes, fungal acne can recur if the underlying conditions that promote its growth aren’t addressed. Proper hygiene, maintaining a balanced skincare routine, and addressing triggers can help prevent recurrence.